The Case:
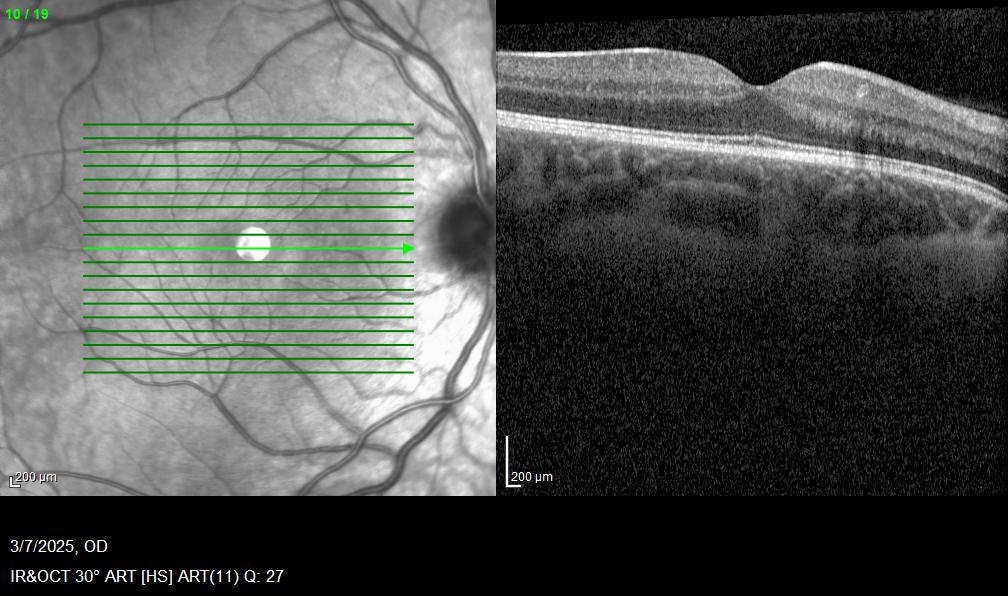
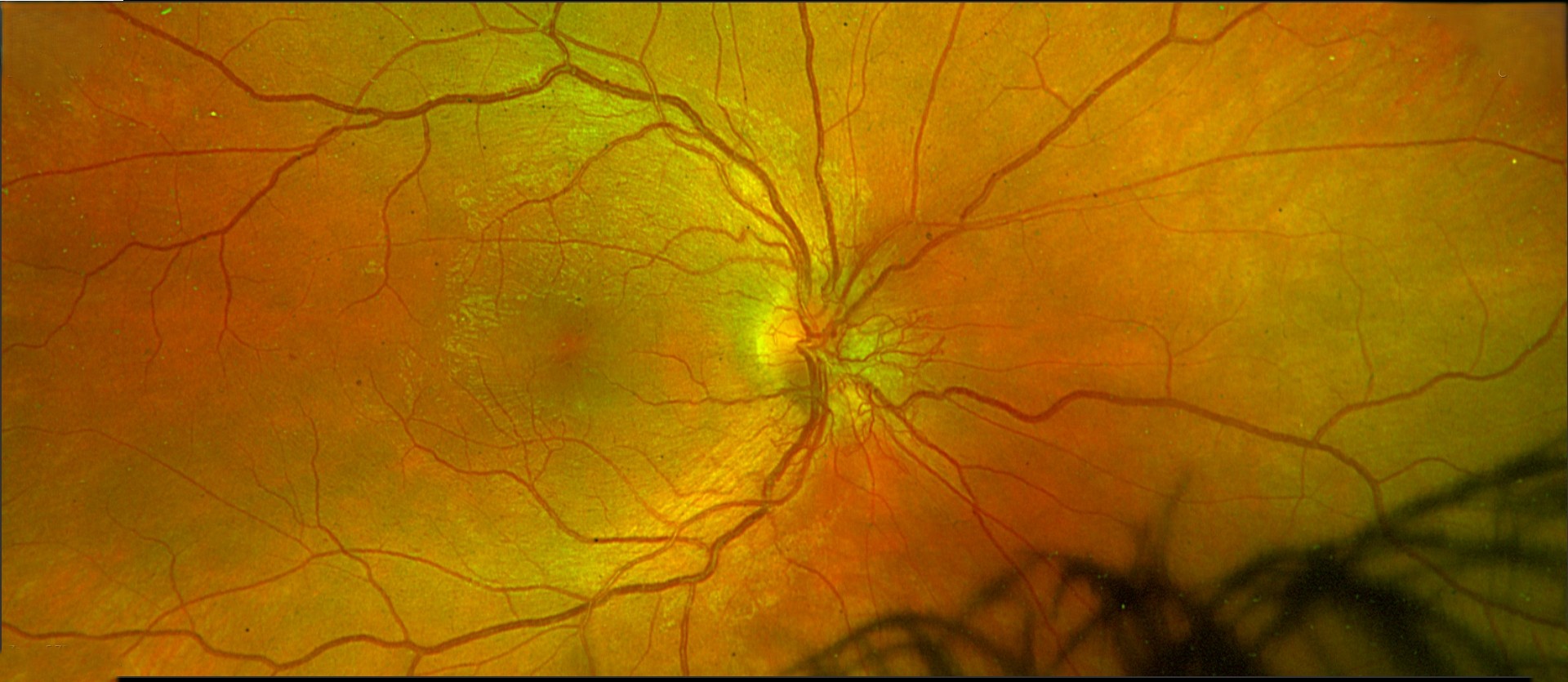
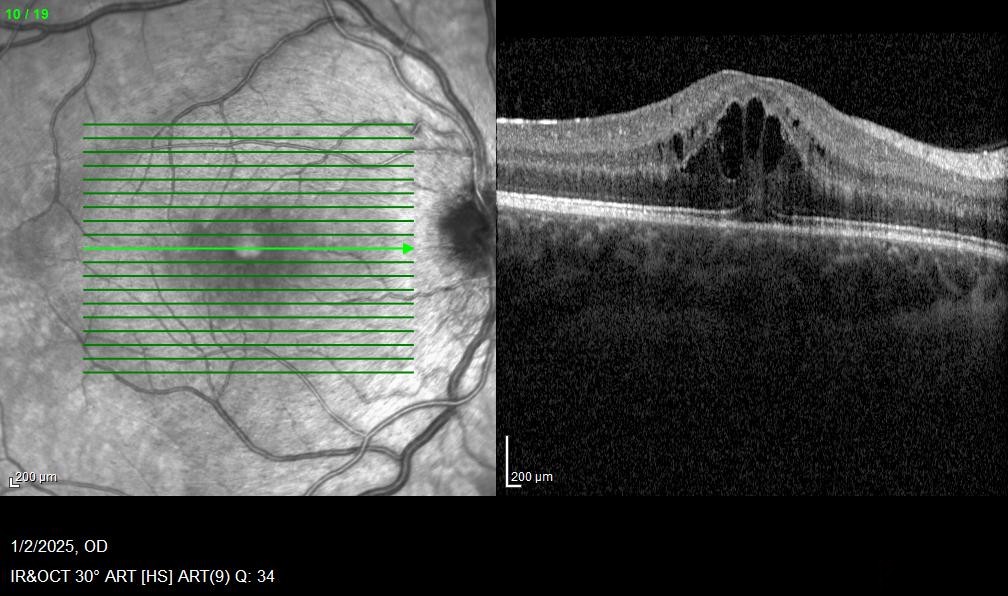
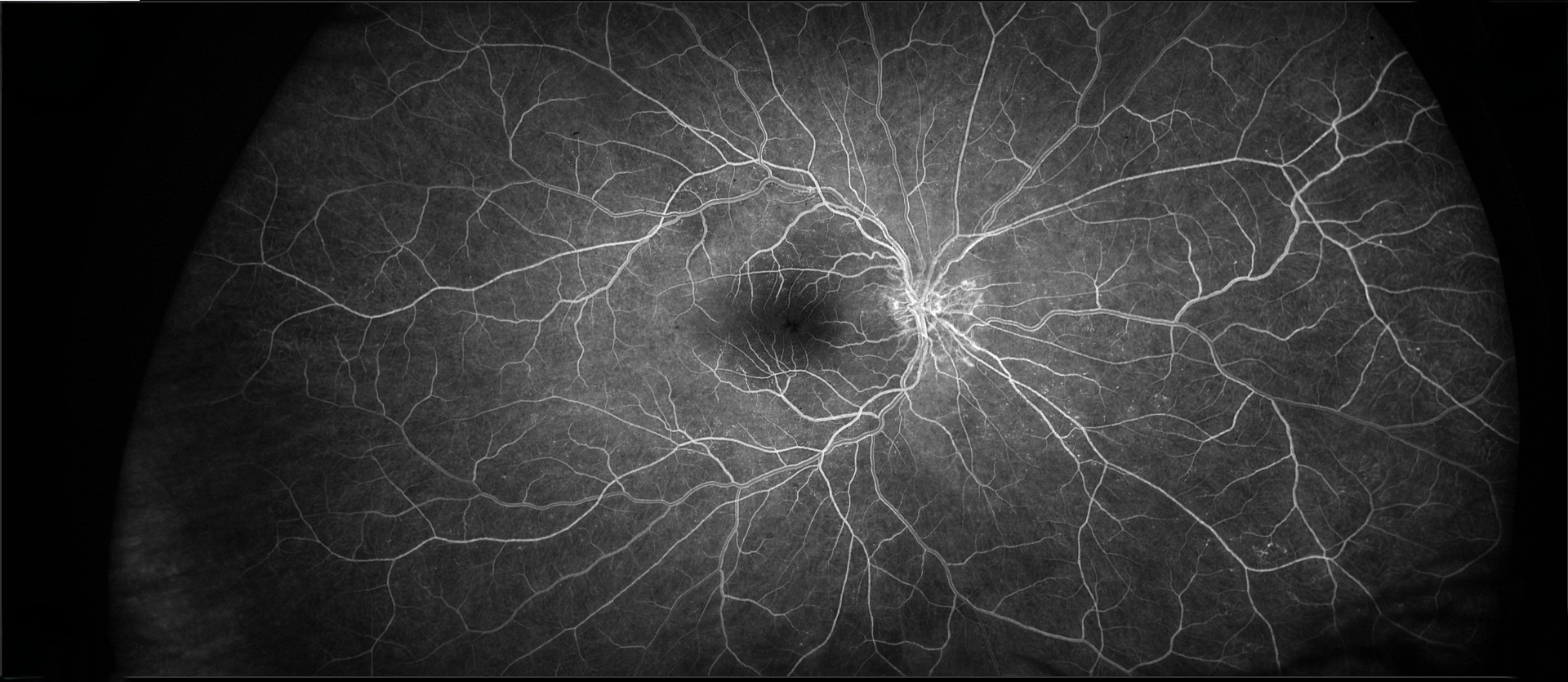
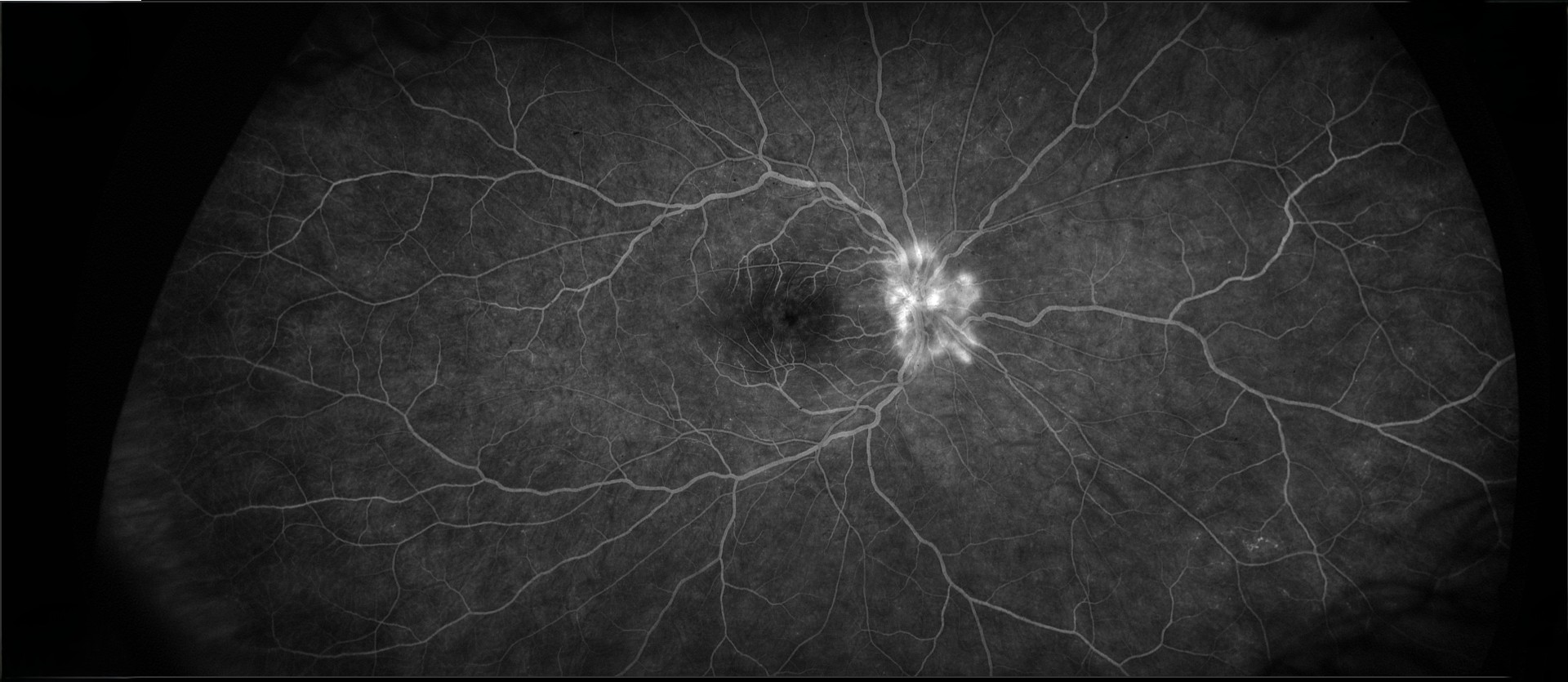
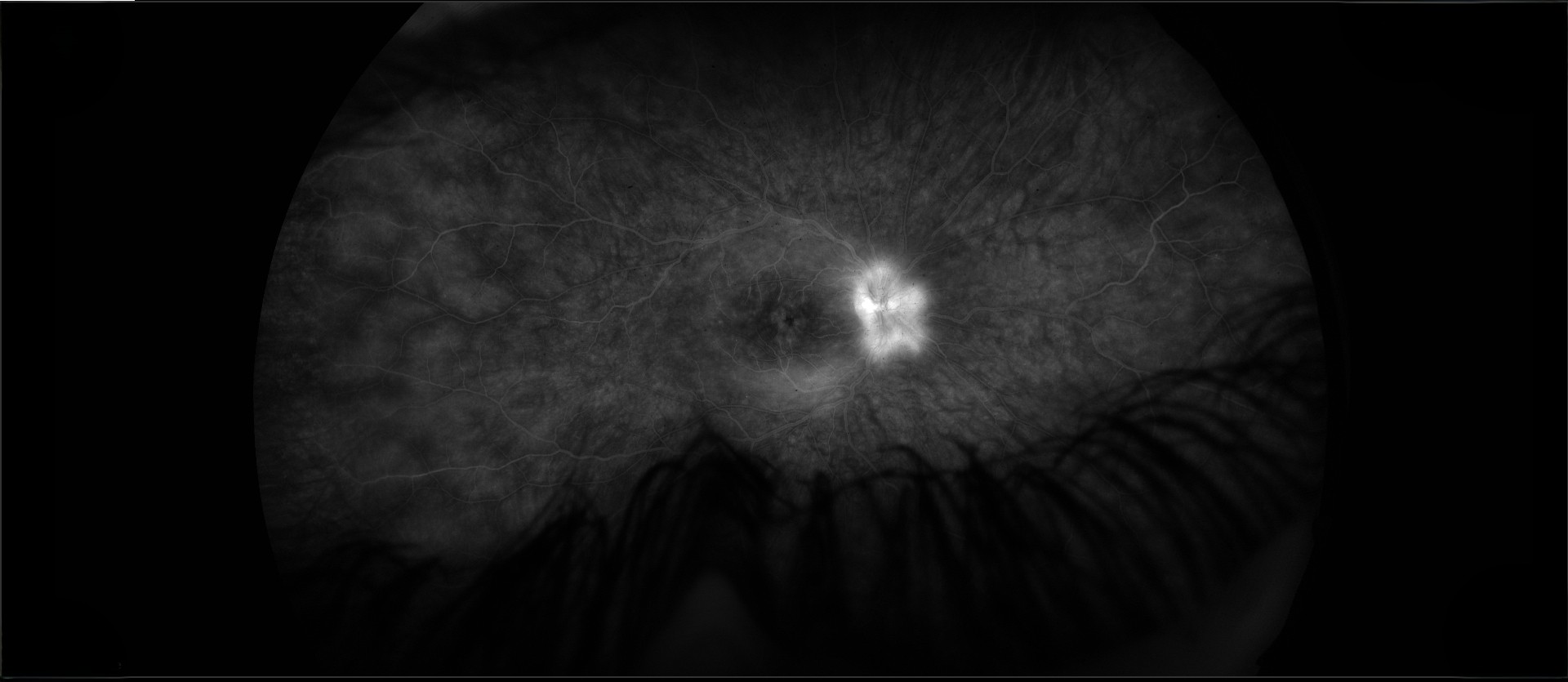
The patient was a 19-year-old woman with intermittent episodes of iritis in the right eye during the past six months who was referred for decreased vision and optic disc changes in the right eye. She had initially presented with severe iritis in the right eye with a hypopyon that responded favorably to topic steroid treatment. She had noticed decreased vision in the right eye for two weeks. She was on prednisonole acetate eyedrops. The visual acuity was 20/40 J1+ OD and 20/20 J1+ OS. There was 1+ conjunctival injection in the right eye, and the anterior chamber had 8 cells per 1 mm2 beam. There were 2+ vitreous cells. Fundus examination revealed disc changes (imaged below) and cystoid macular edema.
Her prior laboratory work-up was remarkable for a weakly positive HLA-B27. The C-reactive protein was mildly elevated at 0.78 (normal 0.0-0.3). Other laboratory studies included an unremarkable CBC; normal sed rate, angiotensin converting enzyme, and uric acid; and negative FTA-Abs, Lyme titer, QuantiFERON gold, and rheumatoid factor.
What was the likely cause of the disc changes and macular edema? What treatment would you recommend?