Answer:
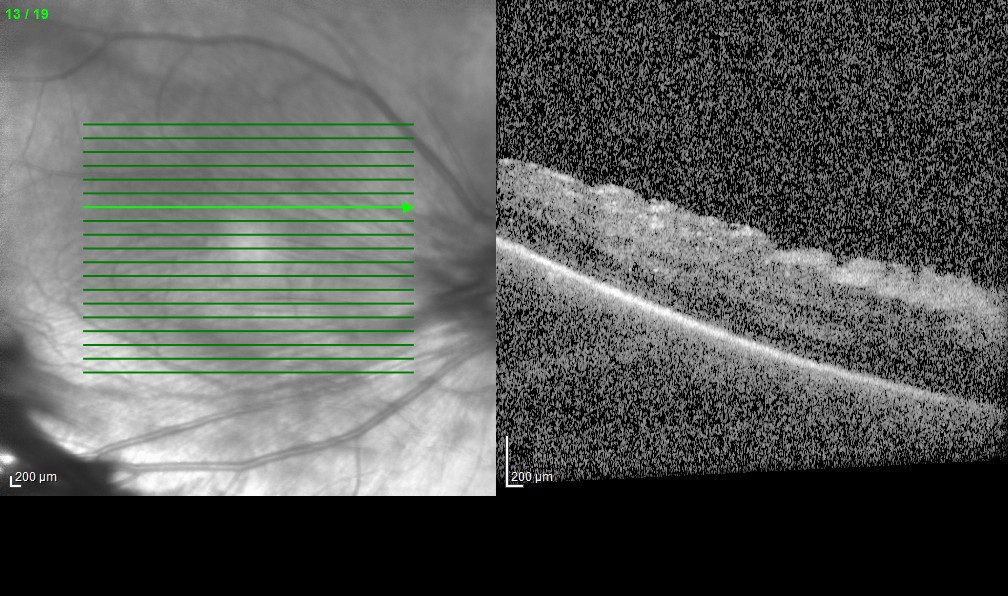
The fundus photograph of the right eye was somewhat blurred by the PSC. In the right eye, there was fibrosis around the optic disc and there was extensive preretinal fibrosis in the temporal periphery extending to the temporal macula. The left eye had mid-peripheral temporal deep pigmentary changes and there appeared to be temporal peripheral nonperfusion. There was severe temporal dragging of blood vessels in right eye and mild temporal dragging in the left eye, which are more readily apparent on fluorescein angiography (FA). FA also revealed peripheral nonperfusion, right eye much more than left, and focal areas of neovascularization in the right eye. In the temporal midperiphery of the left eye, there was early hyperfluorescence without late leakage of fluorescein dye, consistent with a window defect due to RPE disruption. OCT of the right eye revealed surface wrinkling consistent with an epiretinal membrane and mild diffuse edema, while the left macula appeared normal.
This patient had findings resembling retinopathy of prematurity, but she was born full-term. The most likely diagnosis was familial exudative vitreoretinopathy (FEVR), which often has autosomal dominant inheritance with high penetrance and variable expressivity. Mild FEVR manifests with peripheral cystoid degeneration and vitreous traction. More severe disease can show peripheral avascularity, straightening of blood vessels, neovascularization, preretinal fibrosis, and traction detachment. Retinal and subretinal exudation may also occur. These patients are at risk for developing rhegmatogenous retinal detachment, and our patient had an RD in the right eye about one year later.
Several genes have been associated with FEVR, but our patient has not yet had genetic testing. Early laser retinopexy of nonperfused retina might reduce the risk of neovascularization, traction, and/or rhegmatogenous retinal detachment.
Reference
Ranchod TM, Ho LY, Drenser KA, Capone Jr A, Trese MT. Clinical presentation of familial exudative vitreoretinopathy. Ophthalmology 2011;118:2070-5.


%20edited.jpg)
%20edited.jpg)