Answer:
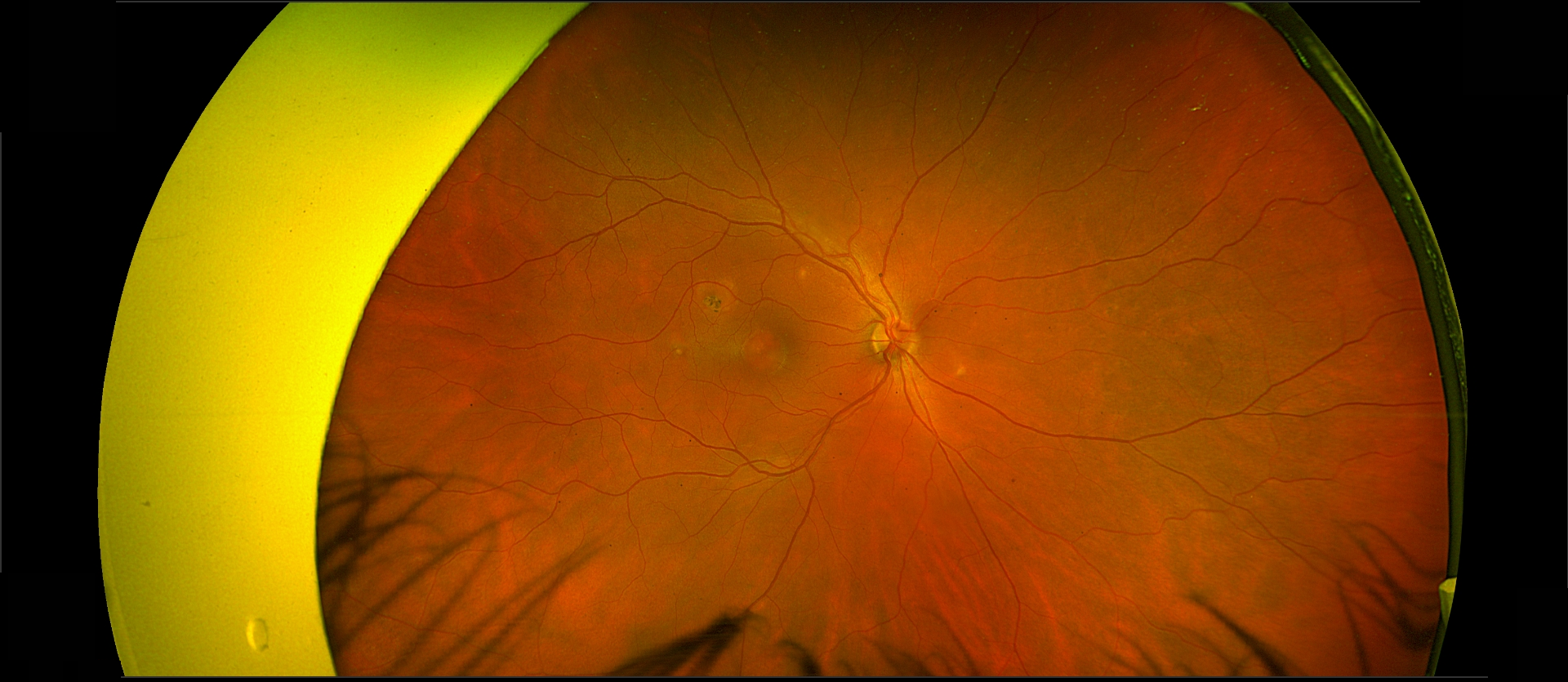
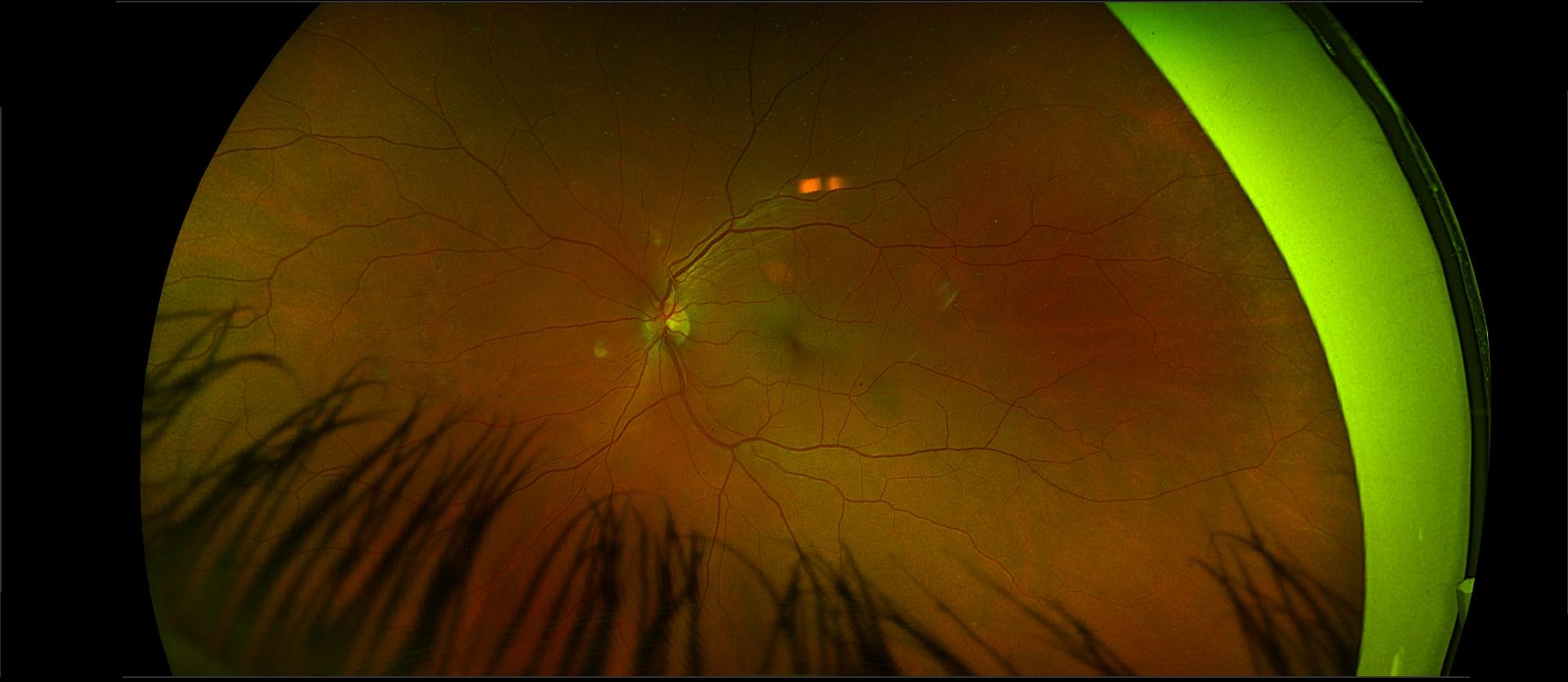
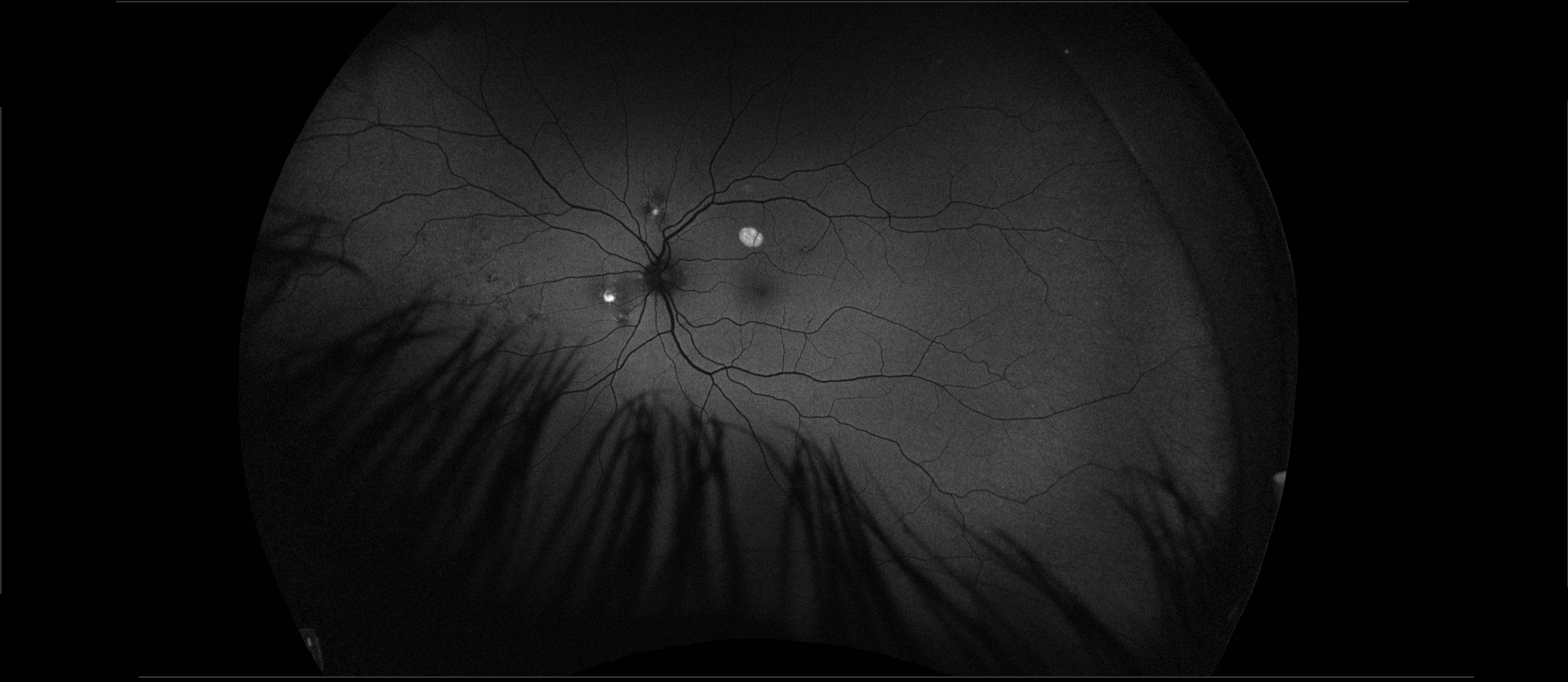
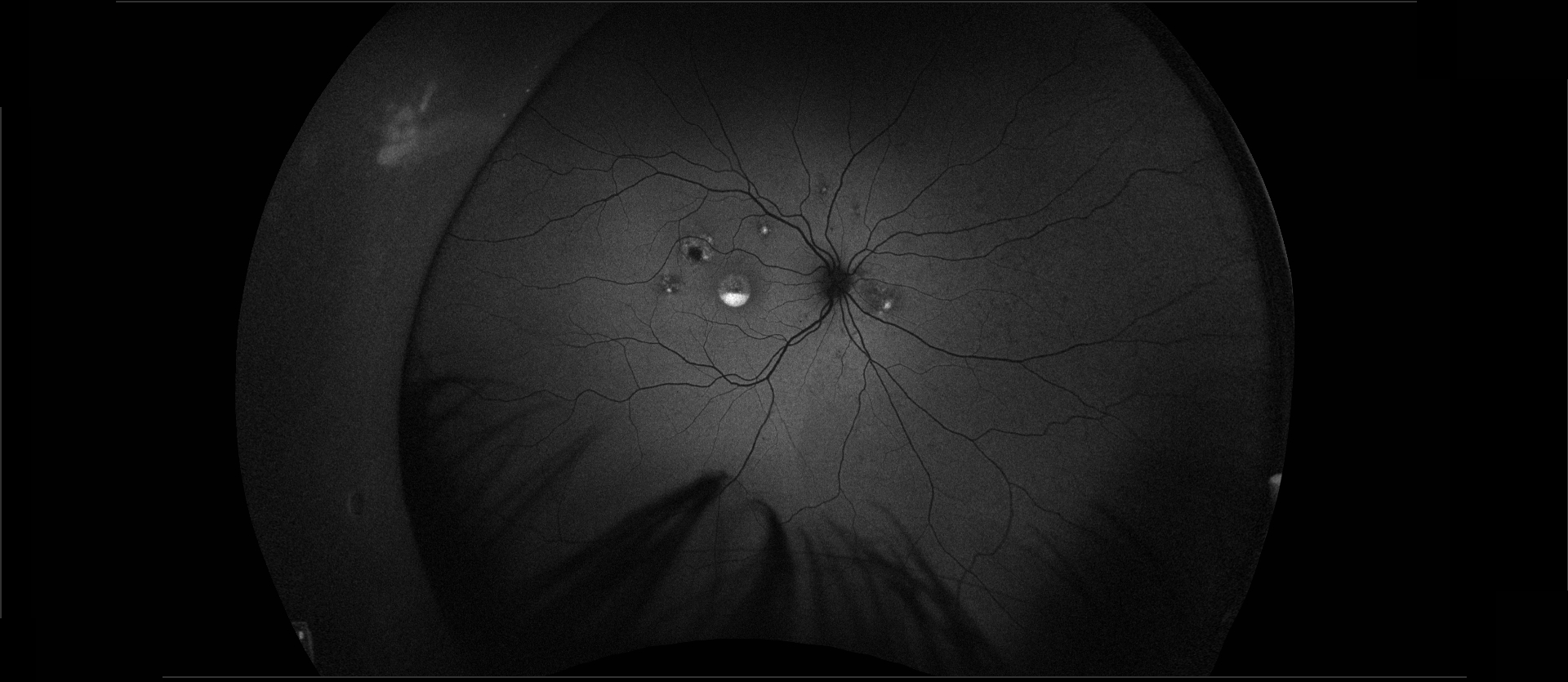
Fundus photography of the right eye reveals a lesion resembling a blister in the central macula, a round chorioretinal scar superotemporal to the fovea, a small scar temporal to the fovea, and three small white spots in the posterior pole. The left eye shows a light orange–colored round lesion above the fovea and two additional white spots in the posterior pole. Fundus autofluorescence demonstrates hyperautofluorescence of the lightly colored lesions in both eyes, as well as layered hyperautofluorescence of the central lesion in the right eye.
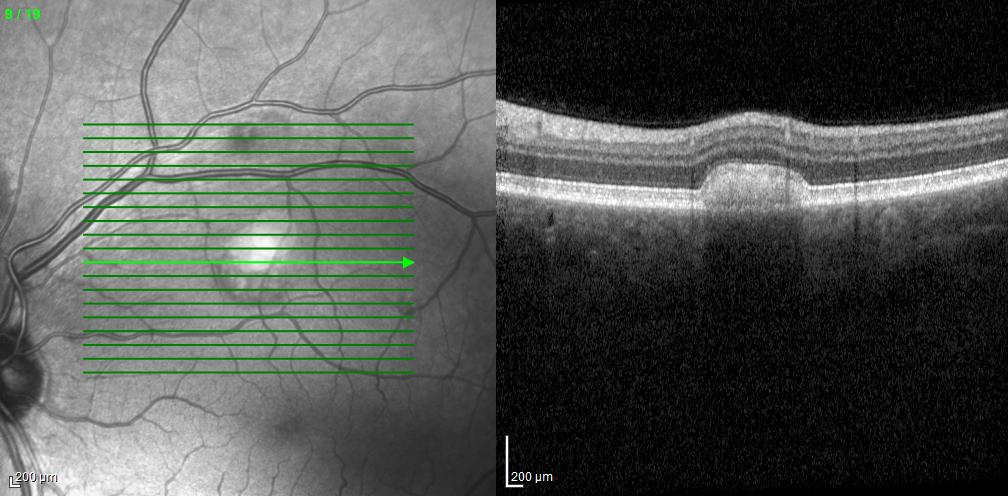
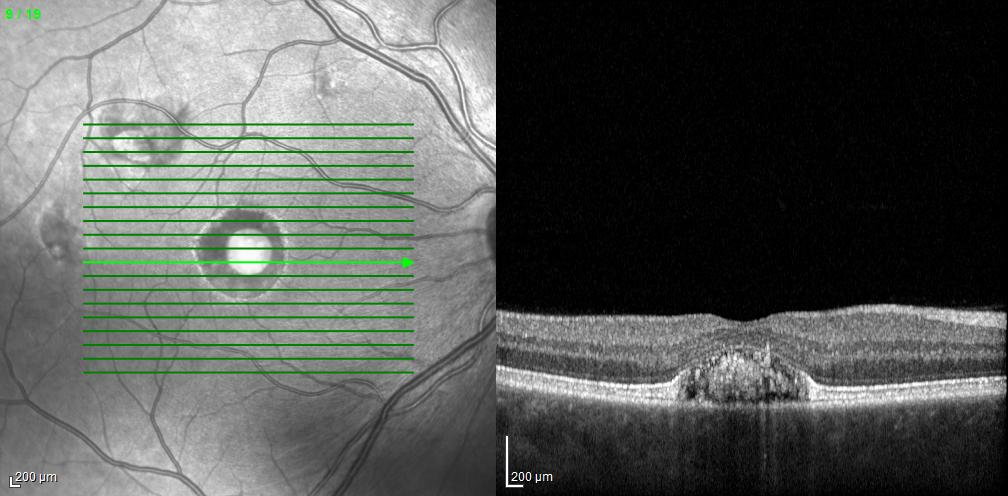
Optical coherence tomography (OCT) through the right fovea reveals a neurosensory detachment with nonreflective material beneath the superior foveal photoreceptors and reflective material centrally. The layered hyperautofluorescence in the right fovea corresponds to this reflective subretinal material. In addition, there is disruption of the retinal pigment epithelium (RPE) and partial loss of the choriocapillaris at the fovea. OCT through the superior macular lesion in the left eye also reveals reflective subretinal material.
Genetic testing identified a heterozygous pathogenic variant in the BEST1 gene, which is associated with autosomal dominant Best disease. The BEST1 gene encodes bestrophin-1, a protein expressed in the RPE that regulates ion transport and calcium signaling.
Before the advent of genetic testing, electro-oculography was useful in diagnosing Best disease. Typically, the Arden ratio is reduced, reflecting diffuse RPE dysfunction, even though the disease appears clinically localized. Our patient’s OCT demonstrates structurally normal RPE and choriocapillaris outside the focal lesions. Full-field electroretinography is usually normal in Best disease, although abnormalities may be detected with pattern or focal ERG.
Vision loss in patients with Best disease most often results from the development of a choroidal neovascular membrane (CNVM). Longstanding neurosensory detachment is often surprisingly well tolerated, although gradual photoreceptor degeneration may occur over time. In this patient, neither the OCT nor the OCT angiogram demonstrated evidence of a CNVM.