Answer:
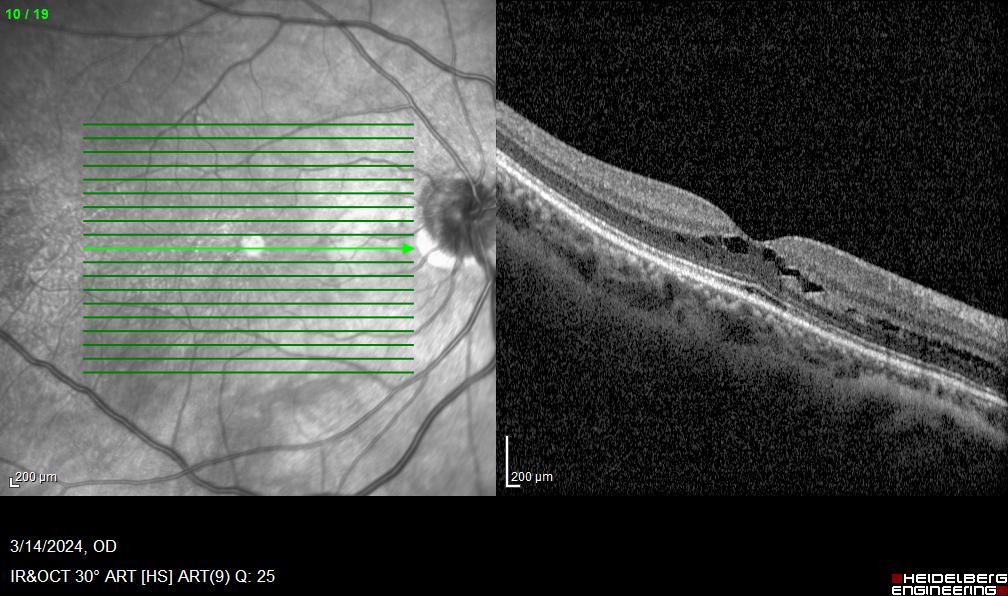
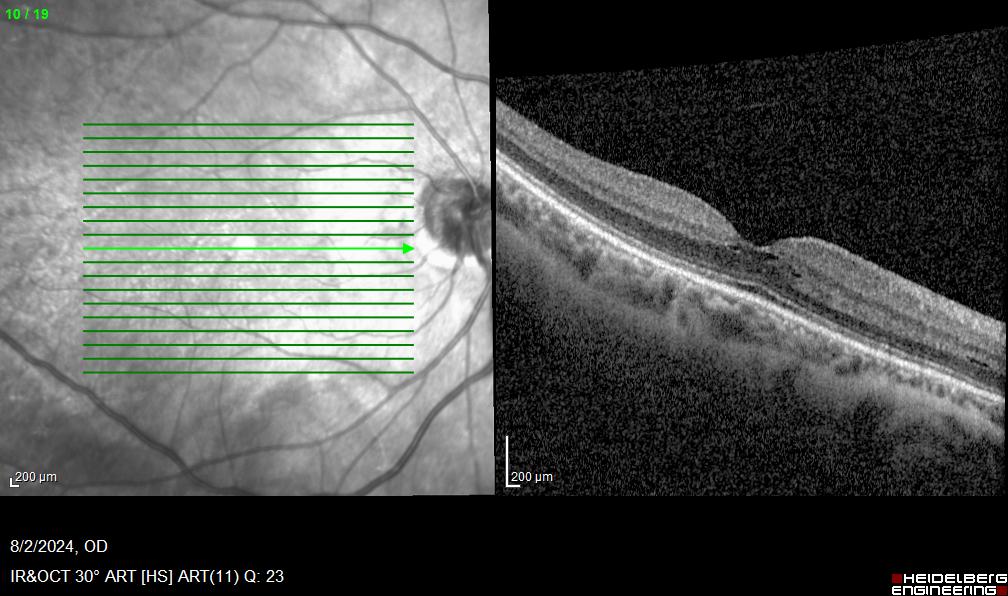
Our patient had schisis-like fluid at the level of the outer plexiform layer in the right eye. This is typical of patients with niacin maculopathy, and our patient had been using 500 mg niacin as well as supplemental magnesium daily for management of her migraine syndrome. The recommended daily allowance for women is 14 mg niacin per day. The supplement was discontinued, and the macular schisis was markedly reduced several months later. There was no change in visual acuity or subjective vision.
There are other diagnostic considerations in a patient with schisis-like intraretinal edema and without any evidence of intraocular inflammation or vasculopathy. Certain immunoglobulin disorders, such as Waldenstrom’s macroglobulinemia or multiple myeloma can present in this manner. X-linked juvenile retinoschisis typically presents with peripheral as well as macular retinoschisis, and the vision is significantly reduced. Stellate nonhereditary idiopathy foveomacular retinoschisis is a rare, bilateral condition which would be in the differential diagnosis for our patient.